The COVID guide: Everything to know about the current state of variants, masking, vaccines and more

Here’s a guide for everything you need to know about COVID-19 — from variant- and case-tracking to the most up-to-date public health recommendations.
Variants
-
What COVID variant is dominant right now? HV.1 now accounts for nearly a third of cases nationwide — more than any other variant in the U.S. A member of the Omicron family of COVID variants, HV.1 was first detected over the summer and appears to share many of the symptoms we’ve come to know from other variants, including fever, cough, stuffy or runny nose, sore throat and loss of taste or smell. EG.5, nicknamed Eris, has been knocked down to second place after being the most dominant variant in early fall, and is responsible for 13.1% of cases. BA.2.86 variant, nicknamed Pirola, is the third-most dominant, accounting for 8.8% of cases nationwide, with cases of the highly mutated variant nearly tripling in the last two weeks. You can follow the latest COVID variant surveillance on the Centers for Disease Control and Prevention website.
-
Are cases currently increasing or decreasing? With less testing and fewer people reporting positive test results to their doctor, case counts are no longer a reliable metric. Instead, officials are using hospitalizations as a key indicator to gauge how prevalent COVID is in the U.S. This week’s national forecast of hospitalizations from the CDC “predicts that the number of daily COVID-19 hospital admissions will remain stable or have an uncertain trend, with 980 to 7,900 daily COVID-19 hospital admissions likely reported on December 25.” And while we’re seeing an increase in illnesses like influenza and respiratory syncytial virus (RSV), CDC Director Mandy Cohen says, “COVID is still the respiratory virus that is putting the most number of folks in the hospital and taking their lives.”
Masks
-
When do I need to wear a mask? Masking at this point is a personal choice, but the CDC suggests using hospital admission levels in your area to determine whether a mask is necessary. You can check hospital admission levels by county here, with data updated by the CDC weekly. The CDC also recommends wearing a mask indoors around others at home and in public for at least 10 days if you test positive for COVID, and wearing a mask around others for up to 10 days if you’ve been exposed to someone who tested positive.
-
Are mask mandates coming back? During an uptick in cases at the end of the summer, some individual schools, businesses and hospital systems decided to bring back temporary masking requirements, but Dr. Anthony Fauci, former director of the National Institute of Allergy and Infectious Diseases, said in September that it’s unlikely federal mask mandates will return. Experts acknowledge that “mask fatigue is real,” and most Americans have ditched masks in public.
Testing
-
Are at-home tests free? As of Sept. 25, every household in the U.S. can order four free rapid COVID tests to be mailed directly to their home. In November, the federal government expanded the program to include four more free tests per household — meaning that if you haven’t taken advantage of free tests since the program started in September, you can now order a total of eight free at-home COVID tests. You can place your order here. Testing will also be available through schools; the U.S. Department of Education recently announced that schools will be able to order free tests “to supply students, families, staff and larger school communities.” And the federal government has additional programs that provide free COVID tests “to uninsured individuals and underserved communities.”
-
How accurate are at-home tests? The Food and Drug Administration says that at-home COVID antigen tests (aka rapid tests) are less precise than molecular tests (i.e., the PCR tests performed at a hospital or clinic), and false negatives may be more likely to happen, especially if the test is taken shortly after infection or when you don’t have symptoms. If you get a negative result on an at-home COVID test, the FDA recommends testing again 48 hours later, even if you don’t have symptoms. PCR tests are still considered the gold standard in COVID testing, but experts believe at-home tests should still be able to pick up newer variants.
-
Can I use an expired test? The Food and Drug Administration has revised expiration dates for some tests to extend them by several months. Follow this link, find your test’s name, click on Extended Expiration Date, and check the lot number on your box to see the new expiration date for your test.
Vaccines
-
Who should get boosted? The CDC recommends that everyone 6 months and older get the updated monovalent vaccine, which became available in September. The updated vaccine targets the XBB.1.5 Omicron strain and is expected to be effective against currently circulating variants. Pfizer’s and Moderna’s vaccines, which use mRNA technology, are approved for anyone 6 months and older. Anyone age 12 and older is eligible for the updated Novavax vaccine, which uses a more traditional protein-based approach. But so far few Americans have taken advantage. As of Nov. 18, just 15.7% of U.S. adults had received the newest COVID shot, according to the latest CDC data.
-
Are vaccines free? COVID vaccines are covered by insurance, Medicare and Medicaid. The federal Bridge Access Program provides free COVID vaccines for uninsured and underinsured adults, and the federal Vaccines for Children program provides vaccines for children at no cost. But the U.S. government is no longer buying and distributing vaccines, which led to a rocky rollout with some canceled appointments as individual doctors offices, pharmacies and insurance companies handle the process themselves.
-
Can you get COVID and flu shots at the same time? Yes. Research shows there’s only a slightly higher chance of experiencing side effects such as pain at the injection site or fatigue, and there’s no decrease in benefit. Experts suggest doing whatever is most convenient, and you can opt for both shots in the same arm or one in each arm.
-
Do vaccine cards matter? Most people no longer need to show that they’ve been vaccinated — unless you’re a health care worker or if you work in a high-risk environment, like a college dorm or nursing home. The CDC has stopped printing vaccine cards, but if you still have your card it’s a good idea to treat it like any other medical record and file it away in a safe place. If you’ve lost your card and want proof of vaccination, some states have registries that include adult vaccines, or you can contact the doctor’s office or pharmacy that administered your vaccine, which can provide digital or paper verification.
What to Know About BA.2.86, the COVID Variant Spreading in the US.
-
Omicron variant BA.2.86 is now making up a larger proportion of COVID cases, according to the CDC.
-
Though BA.2.86 is growing, it seems to be about as transmissible and as severe as most other Omicron variants.
-
With holiday gatherings approaching, people should get vaccinated and take precautions to avoid BA.2.86 infections.
Omicron variant BA.2.86—first detected by the Centers for Disease Control and Prevention in August—appears to be picking up steam in the U.S., the agency announced Monday.
The most recent variant proportions data from the CDC show BA.2.86 (dubbed “Pirola”) making up just under 9% of cases in the U.S.—a threefold increase since two weeks ago when the variant made up 3% of cases. However, these are rough calculations; the CDC estimates that BA.2.86 could make up between 5% and 15% of all cases, currently.
Despite BA.2.86’s increase, the CDC said that the variant “does not appear to be driving increases in infections or hospitalizations” in the U.S. and that current tests, treatments, and vaccines are all expected to be effective against the variant.
In addition to BA.2.86, the CDC noted that cases of another variant—JN.1—are also expected to rise, though it’s still accounting for less than 1% of cases currently. However, both variants are still considered a low public health risk.
Here’s what we know so far about BA.2.86, why it’s causing an increase in COVID cases, and how to best protect yourself during the holiday season.

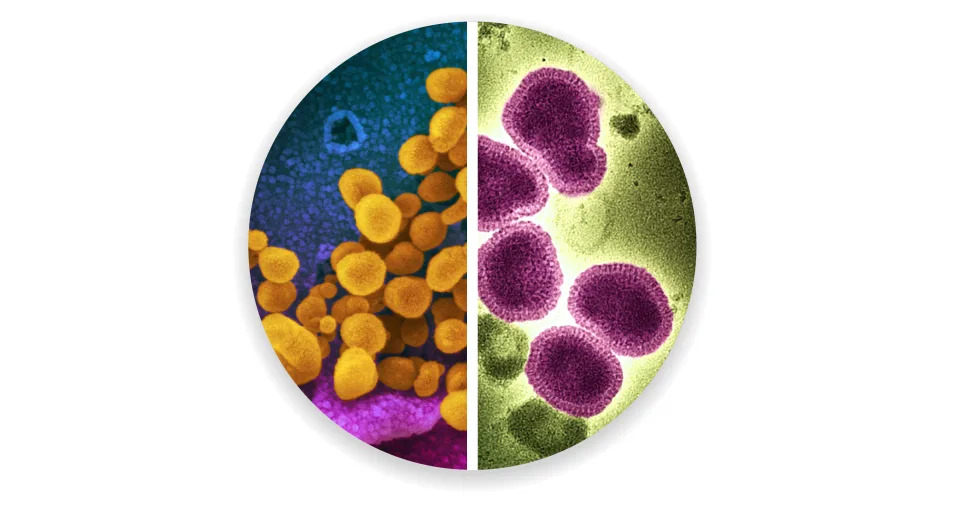
Carol Yepes/Getty Images
How BA.2.86 Compares to Other Variants
All viruses mutate or change in order to survive, including COVID-19, and viruses with these changes are called “variants.”
BA.2.86 appears to have descended from BA.2, known commonly as “stealth Omicron,” which was the dominant variant in the U.S. in early- to mid-2022.
“You can think of [BA.2.86] as a grandchild of Omicron,” William Schaffner, MD, professor of infectious diseases at Vanderbilt University Medical Center, told Health.
Compared to previous variants, BA.2.86 has a large number of mutations—more than 30 mutations that differentiate it from BA.2, and more than 35 mutations than XBB.1.5, another Omicron variant.
These mutations raised concerns among scientists since they could make BA.2.86 better able to evade previous immunity from vaccines or prior infection. It’s because of this that the CDC warned BA.2.86 might be better at causing breakthrough infections, or new cases in people who’ve already had COVID or been vaccinated.
Despite these mutations, BA.2.86 seems to be relatively similar to existing variants in real-world situations.
“This virus is a milder variant, but it looks to be just as contagious as [other Omicron variants],” said Schaffner. “Its infectiousness is about the same, its transmissibility, its contagiousness, and its severity is about the same—namely, it has not produced an increase in severe infections.”
As far as symptoms of BA.2.86 go, the CDC said it’s not currently possible to know if the variant produces symptoms different from other variants. However, symptoms of COVID-19 tend to be similar regardless of variant and often include fever or chills, cough, fatigue, muscle or body aches, and headache.
How to Stay Safe, With the Holidays Fast Approaching
Regardless of which variants are dominant, it’s important that people be extra cautious around the holidays when there’s more opportunity to spread COVID and other respiratory viruses.
“COVID hasn’t disappeared, it’s still with us,” said Schaffner. People may not need to change their behavior or lifestyles, however, the emergence of BA.2.86 is another reminder to be prepared for COVID, especially over the next couple months.
Because BA.2.86 is so similar to other Omicron variants, the updated COVID vaccines and available treatments are expected to be effective against it.
“If you haven’t been vaccinated—and so many people have not yet—there’s still time to get vaccinated,” said Schaffner. “And while you’re at it, get your flu shot, too.”
This is true for everyone, but especially for those who are at an increased risk, such as older people or those with chronic underlying conditions, he added.
“Please be updated with your vaccines and if you’re out in those group activities, think about getting your mask out again, being a little bit extra careful,” he said.
Whether it’s a religious gathering, family party, or other wintertime event, these are occasions that “[COVID] loves, because that will facilitate the transmission of the virus,” said Schaffner.
'Tis the season: What to know about rise in COVID-19 cases, how to stay safe.
Cases of COVID-19 continue to spike, with the frequency of some variants rising quickly.
The Center for Disease Control and Prevention’s Nowcast variant tracker posted on Nov. 27 shows that the BA.2.86 variant – a mutated COVID strain previously thought to be uncommon – is projected to account for nearly one-tenth of circulating viruses. Two weeks ago, the variant made up 3% of cases. These figures are based on estimates of circulating variants.
Similar to other viruses, COVID constantly changes through mutations, making it easier for the virus to spread or resist medicines and vaccines.
COVID cases in Delaware

The Delaware Division of Public Health’s Coronavirus Data Dashboard shows that Delaware has 341,196 total positive cases of COVID as of Nov. 29. Of those cases, 306, 298 are confirmed, 34,898 are probable and 6,416 were documented in residents of long-term care facilities.
New Castle County accounts for the highest number of positive cases at 193,222, followed by Sussex County with 81,255 and Kent County with 66,234.
In the past week, New Castle County saw 205 new positive cases, Sussex County saw 131 new positive cases and Kent County saw 84 new positive cases. COVID infections are most prevalent in the 18 to 34 age range, followed by the 35 to 49 age range and the 5 to 17 age range, according to the Coronavirus Data Dashboard.
As of Nov. 29, there are 67.1 current hospitalizations and 7.9 current critical hospitalizations from COVID, according to the dashboard.
To date, there are 3,512 total deaths from COVID-19 in Delaware, with 3,108 confirmed, 404 deemed probable and 1,091 occurring in long-term care facilities. The CDC defines “probable cases” as those meeting certain clinical or vital records criteria and/or lacking a confirmed lab test for COVID.
For COVID vaccines, only 11.4% of the population of Delaware is vaccinated with the updated 2023-2024 dose.
What are the symptoms of COVID? How long do COVID symptoms last?
People with COVID-19 can experience a wide range of symptoms from mild reactions to severe illness. Symptoms may appear two to 14 days after exposure to the virus, according to the CDC.
Possible COVID symptoms include:
-
Cough
-
Fatigue
-
Fever or chills
-
Shortness of breath or difficulty breathing
-
Sore throat
-
Headache
-
Congestion or runny nose
-
Muscle or body aches
-
New loss of taste or smell
-
Diarrhea
-
Nausea or vomiting
As new COVID variants arise, symptoms may change and can vary depending on vaccination status, according to the CDC.

If you have any of the following symptoms, these are emergency warning signs for COVID and the CDC advises you to immediately seek emergency medical attention by calling 911 or calling ahead to your local emergency facility:
-
Trouble breathing
-
New confusion
-
Pale, gray, or blue-colored skin, nail beds or lips, depending on skin tone
-
Persistent pain or pressure in the chest
-
Inability to stay awake
Before getting treated, be sure to notify the phone operator that you are seeking care for someone who has or may have COVID.
Who should get tested for COVID?

COVID tests are available for anyone to take, whether they have symptoms or not.
If you meet any of the following criteria, you should get tested for COVID and self-quarantine at home while you wait for your results, according to the Delaware Division of Public Health:
-
Anyone who has symptoms.
-
Anyone preparing to attend a large gathering should get tested one to two days prior.
-
Anyone exposed to someone confirmed to have COVID; you should get tested after five days.
-
If you have symptoms and get a negative test result, take another test 2 days later.
You should follow the latest CDC guidance for isolation, which includes information about how long you should isolate for, groups you should avoid during and immediately after your COVID-19 infection, and when you can stop wearing a mask.
If your test results still come back negative, there are other viruses going around, including RSV and influenza, so you should stay home until you are no longer feeling sick. Follow the latest CDC guidance for self-testing and isolating.
RSV vaccine supply dwindles: The RSV vaccine is scarce as cases continue to climb. What to know and prevention tips.
How to prevent the spread of COVID
Aside from getting tested for COVID after showing symptoms or potentially being exposed to the virus, the CDC suggests the following actions as ways to help prevent the spread:
-
Move indoor activities outside, where virus particles do not build up in the air outdoors as much as they do indoors.
-
Get tested for COVID even if you don’t have symptoms or a recent exposure concern. It can help you make informed decisions about your actions.
-
Stay up to date with COVID vaccines, especially if you have a weakened immune system.
-
Wear a mask or respirator to block droplets and particles you breathe, cough or sneeze out. Be sure that the mask you choose fits correctly by covering your mouth and nose and fitting closely to your face.
-
Increase space and distance between yourself and others when in public.
-
Improve ventilation by opening windows; increasing air filtration and frequently changing air filters in your heating, ventilation and air conditioning system; using portable high-efficiency particulate air cleaners; turning on exhaust fans; and turning your thermostat to “on” instead of “auto” to ensure continuous airflow and filtration.
If you are unable to isolate yourself from someone in your home or must care for someone who has tested positive for COVID, properly wash your hands frequently, wear a high-quality mask and keep your distance when possible.
Planning to get the COVID vaccine soon? The Division of Public Health recommends getting vaccinated at least two weeks before traveling to allow the full effects of the vaccine to develop in your body for maximum protection.
How to get tested for COVID in Delaware

Aside from at-home testing kits, available for free from the government or for purchase at local retailers, your best testing option might be to visit free local testing sites near you, which can be found by visiting testinglocator.cdc.gov/.
Once you enter your ZIP code, a list of nearby testing options, along with instructions for scheduling an appointment, will be displayed.
How to get free COVID tests by mail
To place an order for your four free at-home COVID-19 tests, visit special.usps.com/testkits.
The website will prompt you to enter a mailing address and an email and will have a checkout cost of zero. The offer is limited to one order per residential address and includes four individual rapid antigen COVID-19 tests, also referred to as self-tests or over-the-counter tests.
Once the order is placed, an email will be sent to the account used for checkout confirming the order. When the at-home tests are shipped to your home, you will receive a follow-up email with tracking information.
As of Nov. 20, all households are eligible to receive four additional at-home COVID test kits for free following the same instructions, according to an announcement from the U.S. Department of Health and Human Services.
- Questions and Answers
- Opinion
- Story/Motivational/Inspiring
- Technology
- Art
- Causes
- Crafts
- Dance
- Drinks
- Film/Movie
- Fitness
- Food
- Games
- Gardening
- Health
- Home
- Literature
- Music
- Networking
- Other
- Party
- Religion
- Shopping
- Sports
- Theater
- Wellness
- News
- Culture
- War machines and policy

